
Understanding Time Units and Modifiers in Anesthesia Billing
Let’s dive into how time units and modifiers work in specialized anesthesia billing, the common pitfalls to avoid, and how MaxRemind helps ensure your billing process runs smoothly and profitably.
How Anesthesia Billing Time Units Are Calculated
The formula looks like this:
Base Units + Time Units + Modifying Units) x Conversion Factor = Total Reimbursement
- Base Units: Every anesthesia procedure is assigned a set number of base units by the American Society of Anesthesiologists (ASA). These represent the complexity of the service.
- Time Units: For every 15 minutes of continuous anesthesia care, one time unit is added. So if a surgery takes 90 minutes, that’s 6 time units.
- Modifying Units: Sometimes, physical status modifiers or emergency indicators may add additional units.
- Conversion Factor: This is a dollar amount set by Medicare or private payers that converts total units into billable dollars. It varies by state and payer, for example, the 2025 Medicare conversion factor might be lower in New York than in Florida.
Pro Tip: Accurate start and end times must be documented and must match what’s recorded in the anesthesia record or EHR. Any mismatch can lead to denied claims during audits.
Real-World Example:
A patient undergoes a laparoscopic appendectomy in a California hospital.
- Base Units (per ASA): 6
- Time Units: 75 minutes = 5 units
- Total Units: 11
- Conversion Factor (Medicare CA 2025 estimate): $22.75
- Total Reimbursement: 11 x $22.75 = $250.25
Key Anesthesia Modifiers You Need to Know
Here’s a breakdown of the most essential anesthesia modifiers:
| Modifier | Description |
|---|---|
| AA | Anesthesia services are personally performed by an anesthesiologist |
| QK | Medical direction by an anesthesiologist of 2–4 concurrent cases |
| QY | Medical direction by an anesthesiologist of one CRNA |
| QX | CRNA service with medical direction |
| QZ | CRNA service without medical direction |
| AD | Medical supervision of more than four procedures concurrently |
Why do modifiers matter?
- Modifiers Define Roles: Whether the service was performed independently or under direction.
- Modifiers Affect Reimbursement: CRNAs billing under QZ (no supervision) might be reimbursed differently than under QX (with direction).
- Modifiers Ensure Compliance: Medicare and commercial payers require accurate use of modifiers to determine payment.
Common Mistakes in Anesthesia Billing
Top Mistakes Include:
- Rounding time units inaccurately (e.g., rounding up minutes without documentation)
- Using the wrong modifier or omitting it entirely
- Failing to document concurrency for anesthesiologists managing multiple cases
- Missing payer-specific requirements, some commercial payers differ significantly from CMS
- Incorrect start/end times that don’t match the anesthesia record
Why Accurate Anesthesia Billing Matters
- Delayed cash flow due to denials and rework
- Audit exposure from Medicare or private payers
- Lost revenue from under-billing or incorrect units
- Burnout from administrative overload
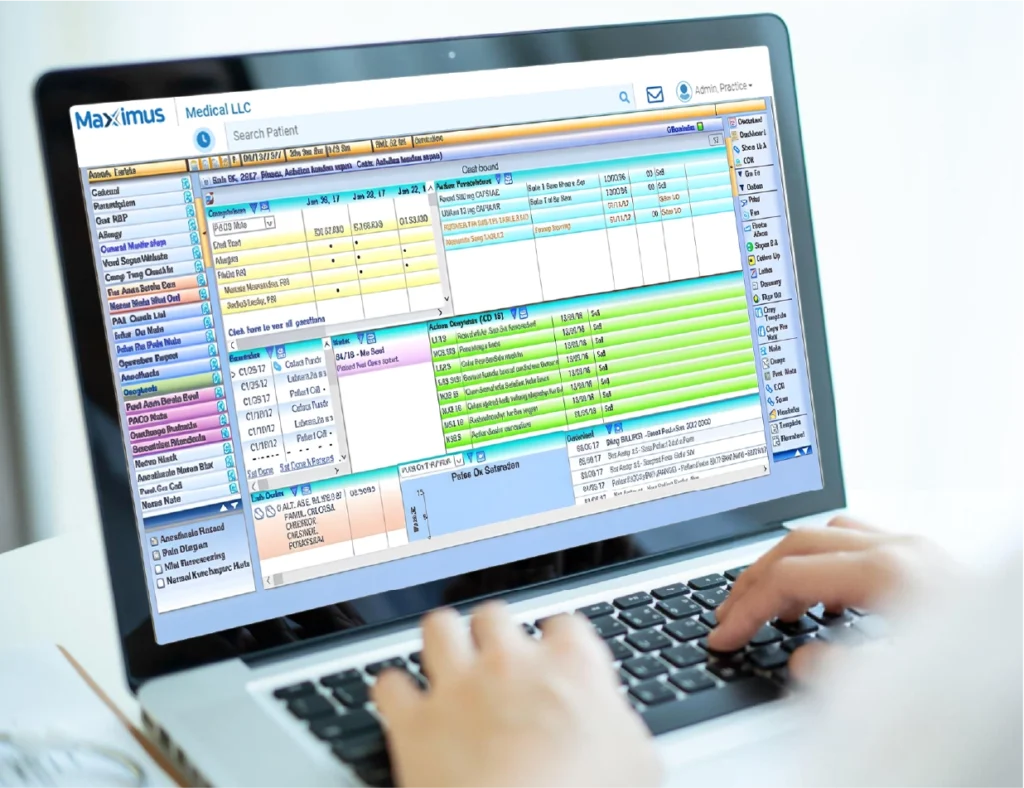
How MaxRemind Supports Anesthesia Billing
MaxRemind understands the intricacies of time-based billing in anesthesia and modifier-heavy workflows. Our team supports hospitals, surgical centers, and group practices across the U.S., offering end-to-end anesthesia billing solutions that reduce denials, ensure compliance, and maximize reimbursements.
Here’s how we do it:
Smart Tech & Trained Experts:
- Time-stamped EHR syncing: We track exact anesthesia time, ensuring proper time unit capture.
- Modifier auto-checks: Claims are flagged if modifiers are missing or mismatched.
- Concurrency monitoring: Real-time alerts if an MD is supervising too many simultaneous procedures.
- Custom payer rule mapping: Our team stays current with each payer’s unique guidelines.
Transparent Performance Metrics:
- Real-time dashboards
- Clean claim rates
- Denial trends and resolutions
- Payer reimbursement reports

Simplify the Complex with MaxRemind
Ready to get started?
- How are anesthesia time units calculated?
-
Time units are determined by dividing the total minutes of anesthesia by 15. One unit = 15 minutes. Start and end times must be documented precisely.
- What are the most commonly used anesthesia modifiers?
-
The most commonly used modifiers are AA, QZ, QX, QK, QY, and AD, each indicating the role of the provider and supervision level.
- What’s the difference between AA and QZ modifiers?
-
Modifier AA is used when an anesthesiologist personally performs the case. QZ applies when a CRNA performs the anesthesia without MD supervision.
- How can I avoid anesthesia billing denials?
-
Ensure accurate time tracking, appropriate modifier use, concurrency documentation, and compliance with payer-specific guidelines.
- Does MaxRemind offer anesthesia billing services?
-
Yes. MaxRemind provides end-to-end anesthesia billing solutions, including time-unit tracking, modifier validation, EHR integration, denial management, and regional compliance support.

