
Thyroid, Diabetes, and Hormone Billing – A Complete Guide for Endocrinologists
Why Endocrinology Billing Requires Special Attention
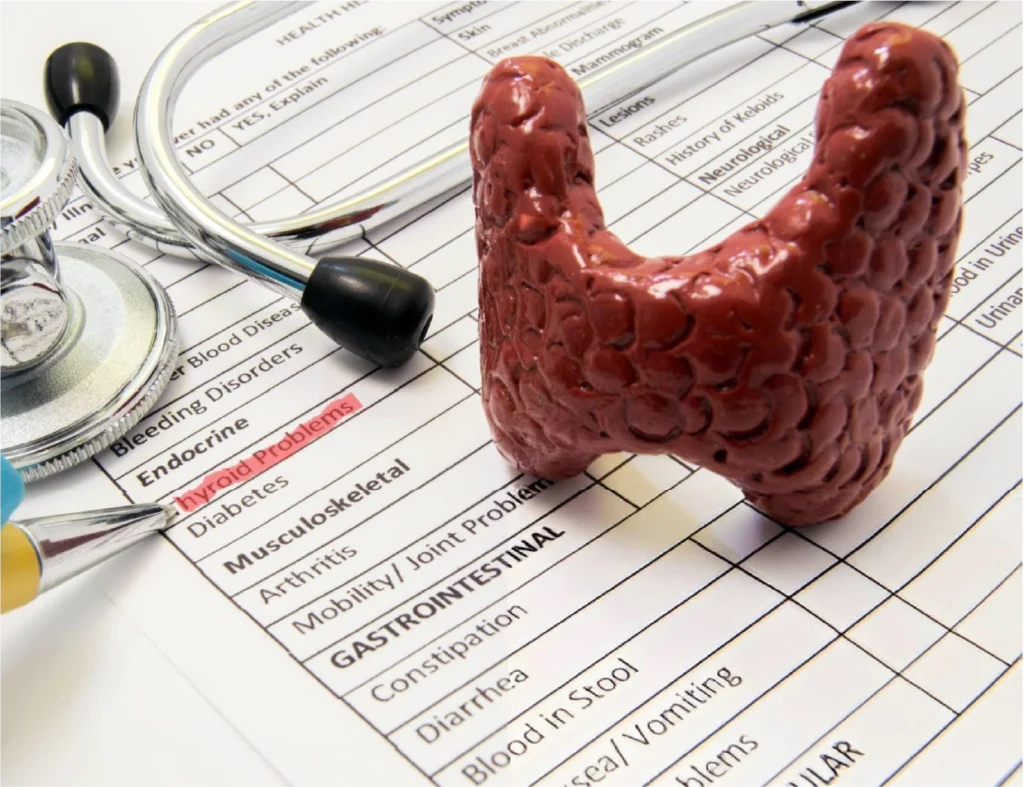
Thyroid Disorder Billing: Essential Codes and Documentation
Thyroid dysfunction is among the most frequently encountered issues in endocrinology. Conditions such as hypothyroidism, hyperthyroidism, thyroid nodules, and autoimmune thyroiditis require both diagnostic evaluation and long-term care. Proper billing starts with selecting the correct CPT and ICD-10 codes and ensuring your documentation supports medical necessity.
Common CPT codes for thyroid-related testing include:
| CPT Code | Description |
|---|---|
| 84436 | Thyroxine, total |
| 84439 | Thyroid Stimulating Hormone (TSH) |
| 84443 | Free T4, direct |
| 76536 | Ultrasound of soft tissues of the neck, commonly used for thyroid imaging |
| 10021 or 10022 | Fine needle aspiration biopsy, with or without imaging guidance |

Diabetes Billing: Managing a Chronic Disease
Useful CPT and HCPCS codes for diabetes care include:
| CPT and HCPCS codes for diabetes | Description |
|---|---|
| 99213 AND 99214 | Follow-up E/M visits depending on complexity |
| 95250 | CGM sensor placement and training |
| 95251 | The interpretation of CGM data |
| G0108 | Individual DSMT sessions |
| G0109 | Group DSMT sessions |

In addition to coding, make sure to thoroughly document coexisting conditions such as diabetic neuropathy (E11.40), nephropathy (N18.9), or retinopathy (H36.0). This helps to paint a full clinical picture and supports the medical necessity of the services provided. For Medicare patients with multiple chronic conditions, CCM billing codes such as 99490 (20 minutes of non-face-to-face care per month) or 99487 (for more complex care management) can be used. However, you must obtain patient consent and maintain detailed time logs and care plans in the medical record.
Hormone Therapy Billing – Medical Necessity vs. Elective Care
Common lab and procedure codes associated with hormone therapy include:
| Lab and Procedure Codes | Description |
|---|---|
| 84403 | Total testosterone |
| 82670 | Estradiol |
| 80415 | Gonadotropin panel (LH and FSH) |
| 82570 | Creatinine, often ordered to interpret hormone lab results |

Telehealth and Remote Services in Endocrinology
Telehealth codes commonly used include:
| Telehealth Codes | Description |
|---|---|
| 99421 to 99423 | Online Digital E/M services |
| 99457 AND 99458 | Remote physiologic monitoring, such as CGM device management |
| 99201 to 99215 | Modifier 95 for real-time audio-video consultations |

Best Practices to Avoid Billing Errors and Denials
- Always verify insurance coverage and authorization requirements for tests, therapies, and procedures
- Ensure documentation supports medical necessity with lab results, physical findings, and patient-reported symptoms
- Use modifiers appropriately, such as modifier 25 for a separately identifiable E/M service on the same day as another procedure
- Maintain up-to-date billing software and coding references, especially with CMS annual changes
- Monitor common denial reasons and create workflows to address them proactively
Conclusion
Need expert help optimizing your endocrinology billing process?
- What CPT codes are used for diabetes management visits?
-
Codes 99213 and 99214 are used for standard follow-up visits depending on the complexity. If you are managing CGM or insulin pump settings, codes 95250 and 95251 may also apply.
- Can endocrinologists bill for chronic care management?
-
Yes, if the patient has two or more chronic conditions, you can use CPT codes like 99490 and 99487. Just ensure you document consent, time spent, and care coordination activities.
- What ICD-10 codes are commonly used for thyroid disorders?
-
Some frequently used codes include E03.9 for unspecified hypothyroidism, E05.00 for thyrotoxicosis without crisis, and E04.1 for a nontoxic single thyroid nodule.
- Is hormone replacement therapy covered by insurance?
-
Yes, but only if it is medically necessary. Treatments for testicular failure or menopausal symptoms are typically covered, while anti-aging or performance-enhancing hormone therapies are not.
- How do I bill for endocrinology telehealth visits?
-
You can use standard E/M codes with modifier 95 for real-time video consults. For online patient interactions, use time-based codes 99421 to 99423 and ensure detailed documentation of time and clinical input.

