
How Automation & AI Are Reshaping Revenue Cycle Management for Physician Practices in the United States
The State of RCM in US Healthcare: A System Under Immense Pressure
High Denial Rates
Recent US industry reports show that claim denial rates have grown by more than 20% in the last five years. Many of these denials stem from preventable issues – eligibility errors, coding inconsistencies, missing documentation, and front-end mistakes.
Staffing Challenges
The United States continues to face a severe shortage of experienced medical billers and coders. Practices are struggling to hire and retain qualified talent, making manual billing processes even more difficult to sustain.
Increasing Payer Requirements
Commercial payers and government payers are tightening policies, adding new documentation standards and prior authorization rules. This makes manual workflows even more complex.
Administrative Burden on Providers
Physicians already spend nearly 50% of their time on administrative tasks. Manual eligibility checks, coding, and claims follow-up add to the burnout problem across US practices.
How AI & Automation Are Transforming Revenue Cycle Management

Automated Eligibility & Benefits Verification
- Verify eligibility in seconds
- Detect changes in patient coverage
- Identify coverage limitations
- Flag missing prior authorization requirements
- Reduce the risk of eligibility-related denials
AI-Driven Medical Coding & Documentation Accuracy
- Higher coding accuracy
- Reduced compliance risk
- Faster documentation-to-claim submission
- Lower workload for coders
Predictive Denial Management & Claims Scrubbing
- Detect high-risk claims before submission
- Identify missing documentation
- Recommend corrections automatically
- Flag payer-specific rules
- Higher clean-claim rates
- Fewer denials
- Faster payments
- Reduced administrative workload
Automated Payment Posting & Reconciliation
RPA for Claims Follow-Up & AR Management
- Monitor claim status
- Follow up with payers
- Update AR buckets
- Trigger actions for staff based on payer response
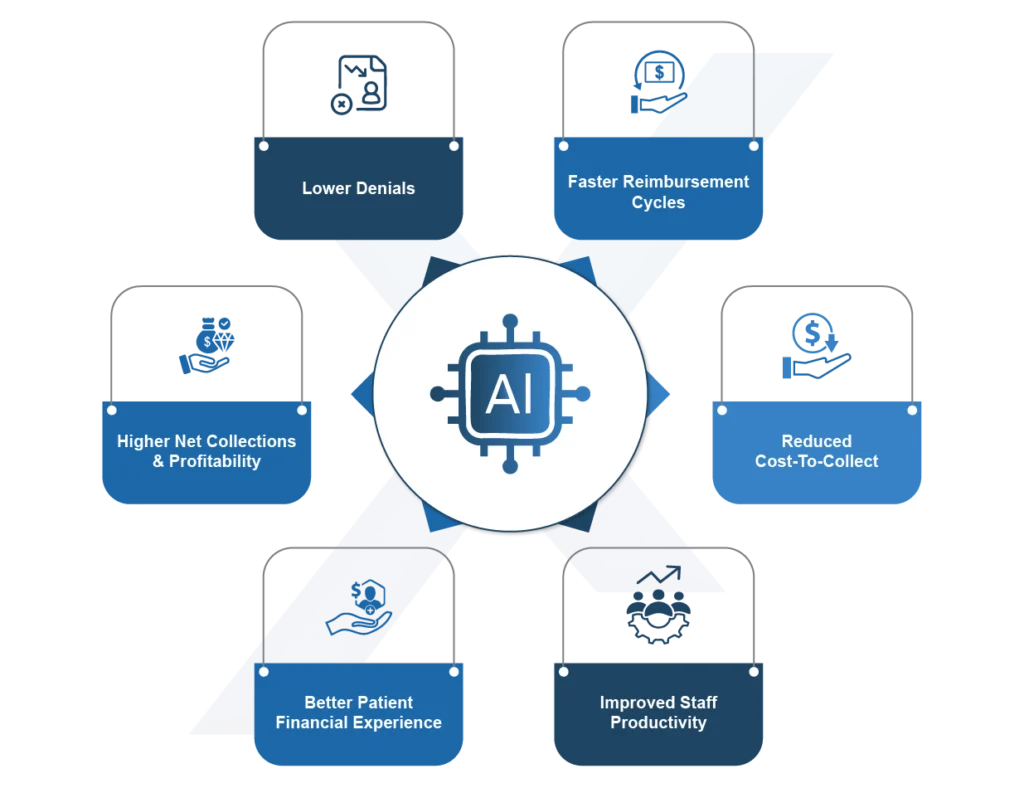
Real-World Benefits for US Physician Practices
-
Lower denials
Thanks to predictive analytics, automated scrubbing, and eligibility verification. -
Faster reimbursement cycles
Clean claims get paid faster – improving cash flow. -
Reduced cost-to-collect
Automation minimizes repetitive manual tasks and cuts administrative overhead. -
Improved staff productivity
Teams focus on complex tasks rather than routine billing processes. -
Better patient financial experience
Accurate eligibility checks, faster billing, and transparent communication improve patient trust. -
Higher net collections & profitability
Optimized revenue cycles lead directly to better financial outcomes for practices.
What Physician Practices Should Prioritize When Implementing AI & Automation
To maximize results, US practices should keep these considerations in mind:
-
Platform interoperability (EHR/PM integration)
Ensure the RCM solution integrates seamlessly with your EHR, practice management system, and clearinghouses. -
Data quality & standardization
AI performs best with clean, structured data. -
Compliance & security
Choose HIPAA-compliant vendors with strong encryption and audit controls. -
Specialty-specific features
Specialties like cardiology, orthopedics, endocrinology, behavioral health, or pain management require tailored RCM workflows. -
Scalability
Choose a solution that supports future practice growth.

Why MaxRemind Is the Trusted AI-Driven RCM Partner for US Practices
MaxRemind is a leading provider of AI-powered medical billing and revenue cycle management services trusted by physician practices, specialty groups, and billing services across the United States.
- Higher clean claim rates
- Lower denials
- Faster reimbursement
- More predictable cash flow
- Reduced operational costs

The Future of RCM Belongs to AI-Powered Practices

Ready to Modernize Your Revenue Cycle? Partner With MaxRemind
- How does AI improve revenue cycle management for physician practices?
-
AI improves RCM by automating complex tasks such as eligibility verification, coding accuracy, denial prediction, and claims follow-up. AI tools identify errors before claims are submitted, reduce the chance of denials, and speed up reimbursement cycles. For larger physician practices and specialty groups, AI significantly improves clean-claim rates and reduces administrative workload.
- Can automation reduce claim denials in medical billing?
-
Yes. Automation is one of the most effective ways to reduce claim denials. Automated systems validate patient eligibility, check documentation completeness, detect missing prior authorizations, and scrub claims using payer-specific rules. This prevents the most common front-end errors. Many practices that implement automated RCM tools report a 30–50% reduction in preventable denials.
- Is AI-based medical coding accurate enough for specialty practices?
-
Absolutely. AI-driven medical coding uses natural language processing (NLP) to analyze clinical notes and assign accurate codes –including specialty-specific codes for cardiology, orthopedics, oncology, neurology, and more. This reduces compliance risks, speeds up coding turnaround times, and supports coders by eliminating repetitive tasks. AI enhances accuracy but does not replace certified coders – it augments them.
- What should healthcare practices consider before implementing AI and automation in RCM?
-
Practices should focus on EHR/PM interoperability, HIPAA-compliant security, data quality, specialty-specific support, and scalability. Seamless integration with existing systems is crucial for achieving maximum value from AI tools. Choosing a trusted partner like MaxRemind ensures proper implementation, optimized workflows, and ongoing support for long-term success.
- How does MaxRemind use AI and automation to improve revenue cycle performance?
-
MaxRemind integrates advanced AI, machine learning, and RPA technologies to streamline eligibility checks, coding, payment posting, denial management, and AR follow-up. With specialty-trained billing teams and automated tools, MaxRemind helps practices achieve faster payments, lower denials, reduced cost-to-collect, and stronger financial stability. You can also request a Free Practice Audit to identify improvement areas.
