MRI Billing & Prior Authorization: Steps to Prevent Revenue Loss
For radiology billing professionals, imaging centers, and RCM companies, mastering MRI billing is not just about accuracy; it’s about ensuring their work remains sustainable and successful over time. This blog breaks down the essentials of proper MRI billing, outlines the necessary steps for successful prior auth, and explores how AI-powered solutions like MaxRemind can help eliminate common errors and protect your revenue cycle.
Common MRI CPT codes include:
Strategies for managing bundling in IR billing:
| CPT Codes | Description |
|---|---|
| 70551-70553 | Brain MRIs |
| 72141-72142 | Spinal MRIs |
| 73721-73723 | Lower Extremities |
| 73221-73223 | Upper Extremities |
- Use Modifier 26 when billing only for the interpretation (professional)
- Use Modifier TC when billing for the technical component (equipment and setup)
Prior Authorization
When is prior auth required?
- Most commercial insurance plans
- Some Medicare Advantage plans
- Medicaid plans (state-specific)

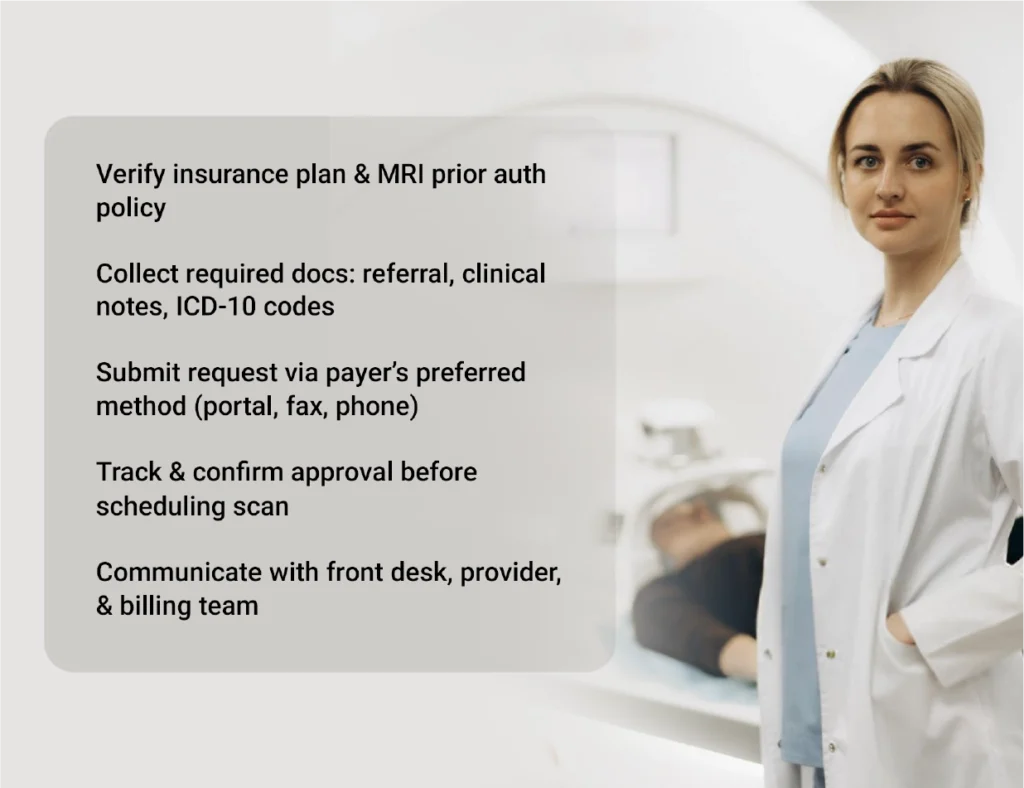
Steps for Successful Prior Authorization
Steps to ensure success:
- Verify insurance plan and policy regarding MRI prior auth
- Gather necessary documentation, including:
- Referral from the ordering provider
- Clinical notes supporting medical necessity
- Relevant ICD-10 codes
- Submit the request through the payer’s preferred method (portal, fax, phone)
- Track and confirm approval before the scan is scheduled
- Communicate across departments to make sure the front desk, provider, and billing team are all on the same page
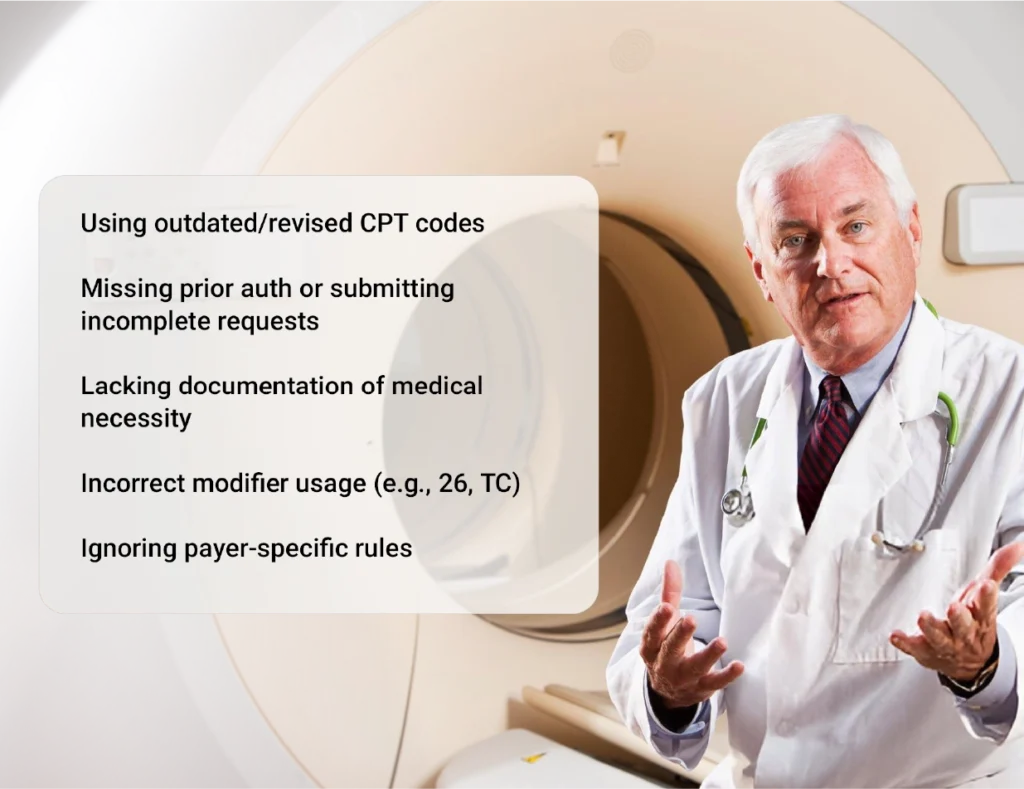
Common Pitfalls in MRI Billing
Some of the most common pitfalls include:
- Using outdated CPT codes that have been revised or replaced
- Failing to obtain prior authorization or submitting incomplete requests
- Insufficient documentation of medical necessity
- Incorrect modifier usage, especially with Modifier 26 and TC
- Not knowing payer-specific rules, which can vary widely across insurance providers
How AI and Technology Can Help Prevent Revenue Loss
- Automatically check if prior auth is required for a specific payer and procedure
- Alert staff when documentation is missing before claim submission
- Cross-verify CPT and ICD-10 codes to ensure alignment and reduce denials

MaxRemind’s AI-powered RCM tools are designed specifically for diagnostic imaging centers. These include:
- Built-in prior authorization modules
- AI-assisted coding support that flags inconsistencies in real time
- Claim scrubbing engines that identify missing elements before submission
These tools help teams catch problems early, before they become revenue loss events.
Best Practices to Avoid MRI Revenue Loss

Conclusion
Ready to stop revenue loss before it starts?
- What is the prior authorization process for MRI scans?
-
The prior authorization process for MRI includes checking insurance requirements, gathering supporting documentation, submitting an approval request, and waiting for payer confirmation before performing the scan.
- Why do MRI claims get denied by insurance companies?
-
MRI claims often get denied due to missing prior authorization, incorrect CPT codes, lack of medical necessity, or incomplete documentation.
- Do all insurance plans require prior authorization for MRIs?
-
Not all, but many commercial and Medicaid/Medicare Advantage plans require prior auth for MRI. Always check the patient’s benefits before scheduling.
- Can AI help with MRI billing and authorization?
-
Yes, AI can help automate prior auth submissions, flag billing issues, verify eligibility, and reduce manual errors that lead to denied MRI claims.
- What CPT codes are used for MRI procedures?
-
CPT codes for MRI depend on the body part being scanned. Examples include 70551 (MRI brain), 72148 (MRI lumbar spine), 73721 (MRI knee), and more.